Liver cancer is cancer that originates in the cells of the liver. The liver is an organ situated in the upper right portion of the abdomen, beneath the diaphragm and above the stomach. It is one of the major organs responsible for removing toxins from the body. Liver cancer is common in Asian countries such as Hong Kong, Taiwan and Singapore. In the early stages, most patients may not have any specific symptoms.
- Chronic carriers of Hepatitis B virus and Hepatitis C virus
- Those with liver cirrhosis
- Those with Hepatitis B or C related diseases
- Those with a bile duct disease called primary sclerosing cholangitis
- Alcohol abusers (Alcohol abuse can lead to liver cirrhosis)
*People who think they may be at risk should discuss this with their doctor.
Early stage liver cancer may not produce any signs. As the cancer advances to a later stage, it may produce the following symptoms:
- Loss of appetite and weight
- Weakness and fatigue
- Nausea and vomiting
- Abdominal swelling/bloated
- Lump in the abdomen
- Abdominal pain
- Yellowish discoloration of the skin and whites of eyes (jaundice)
*A doctor should be consulted if the above symptoms occur. Screening for liver cancer is still under investigation. However, patients who are in the high-risk* group are often advised to consider regular evaluations with:
- Blood test for alphafetoprotein (AFP) and liver function assessment every 6 months
- Ultrasound scan of liver every 6 months
*People with liver cirrhosis, are hepatitis B carriers or have chronic hepatitis C infection.
If you present with one or more of the above symptoms, your doctor will try to find out if it is caused by liver cancer or something else. You may be asked to do one or more of the following tests.
Blood Tests
Liver function abnormalities may be revealed by conducting blood tests.
Imaging Tests
Ultrasound, Computed Tomography (CT) scans and Magnetic Resonance Imaging (MRI) scans may be performed.
Laparoscopy
In this procedure, a thin, lighted tube with a camera on the tip is inserted through a small incision in the front of the abdomen to examine the liver and other organs. It can help doctors confirm the extent of the cancer.
Biopsy
In a biopsy, a sample of tissue is removed to see if it is cancerous. Different procedures such as a needle biopsy, a laparoscopic biopsy or a surgical biopsy may be performed.
There are different treatments available for liver cancer depending on the stage of the cancer as well as the health of your liver. Treatment options may include:
Surgery
Suitable patients may undergo liver resection surgery which involves the surgical removal of the tumour and surrounding liver tissue from the liver. Patients with small tumours may also be suitable for a liver transplant.
One of the main issues for surgery for advanced liver cancer is the residual functional liver after surgery and here at the NCIS, we have specialised in staged procedures to overcome this obstacle by allowing the healthy liver to hypertrophy before the definitive surgery is carried out to remove the tumour.
As a university surgical unit, we have advanced in the minimally invasive surgical techniques for liver cancer which includes laparoscopic targeted therapies for liver such as radio-frequency ablation and laparoscopic liver resections.
The NCIS provides the full spectrum of liver cancer surgery including liver transplants. A liver transplant is a surgical procedure which involves removing and replacing the diseased liver of the patient with a healthy liver from a donor. Most liver transplant operations use livers from deceased donors, though a liver may also come from a living donor.
Liver-Directed Therapies
- Radiofrequency Ablation
A procedure which destroys the tumour without removing the liver. High-energy beams travel down a thin metal probe that is inserted into the liver and through the tumour. Ultrasound is used to guide the probe into place and the heat that is emitted destroys the tumour.
- Trans-Arterial Chemoembolisation
Chemotherapy is the use of anti-cancer drugs to destroy cancer cells or stop them from dividing. It may be administered as part of a treatment called chemoembolisation. Chemoembolisation involves the insertion of chemotherapy drugs directly into the tumour in the liver, together with a gel or tiny plastic beads to block blood flow to the cancer (embolisation). Embolisation prevents the tumour from growing as it is deprived of blood.
- Selective Internal Radiation Therapy
Selective Internal Radiation Therapy is a technique that involves the use of many tiny beads in delivering extremely high dosages of radiation. The radiation travels directly to the tumour through the hepatic artery. This limits the amount of radiation that the normal tissue in the liver is exposed to.
- NanoKnife Therapy
NanoKnife is a minimally invasive cancer treatment that uses a targeted approach to treating hard to reach tumours at the cellular level. It relies on the body's natural healing ability to replace cancer cells once they are destroyed, so it leaves almost no scarring. NanoKnife works by applying electrical energy directly into tumours. This opens the cell walls of the tumor; the cancer cells die, and healthy tissue remains unharmed. NanoKnife serves as an alternative treatment approach to thermal ablation which kills cells with extreme heat or cold. NanoKnife can destroy tumours that may not be treatable with surgery or radiation therapy. Patients undergo general anesthesia and experience little pain following the procedure. Treatment requires only a brief hospital stay.
Targeted Cancer Therapy
Targeted cancer therapy uses drugs or other substances that block the growth and spread of cancer by interfering with specific molecules involved in cancer growth and progression. A targeted drug called sorafenib may be used to treat patients with advanced liver cancer. Sorafenib targets cancers by stopping them from growing their own blood vessels. As cancer cells need a blood supply to bring nutrients and oxygen, sorafenib may therefore limit the cancer’s ability to develop.
Sorafenib has been demonstrated to prolong survival in patients with advanced HCC, compared with supportive care alone. Sorafenib is an oral treatment and is usually taken twice a day.
NCIS provides a TOTAL liver cancer care treatment approach from early detection techniques to new advanced liver directed therapies to liver surgery and transplants.
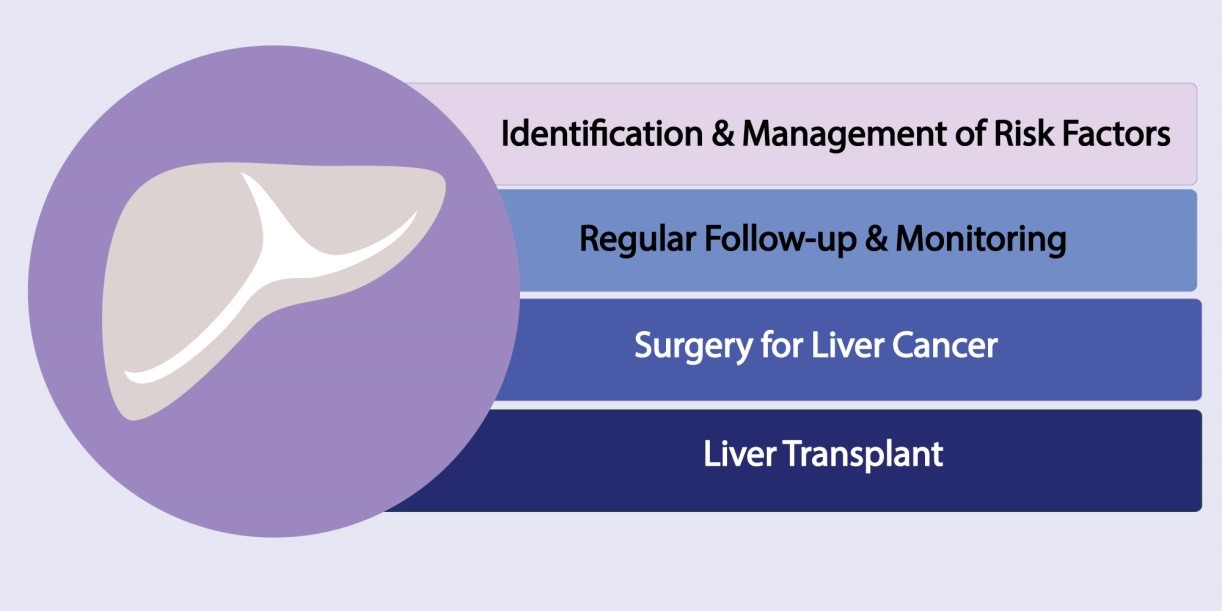
Some key components under the NCIS' total liver cancer care treatment approach include:
Identification and Management of Risk Factors
Our total liver cancer care treatment approach involves identification and management of risk factors for liver cancer. These include screening for Hepatitis B and C infections, liver cirrhosis, early detection of liver cancers and counselling for alcohol dependence. Our comprehensive liver cancer care team includes gastroenterologists and liver physicians who regularly follow-up patients with risk factors and screen them regularly for early detection of any possible liver cancers.
Regular Follow-up and Monitoring
Treatment for and monitoring for viral hepatitis, comprehensive management team for liver cirrhosis including counselling sessions are available at the NCIS.
Once a new liver cancer is detected the cases are subjected to extensive review and discussion by our Multi-Disciplinary Tumour Board which includes surgeons, liver specialists, radiologists and oncologists who will cater the best treatment modality suitable for each case.
Surgery for Liver Cancer
Suitable patients may undergo liver resection surgery which involves the surgical removal of the tumour and surrounding liver tissue from the liver.
One of the main issues for surgery for advanced liver cancer is the residual functional liver after surgery, however, at the NCIS, we are specialised in staged procedures to overcome this obstacle by allowing the healthy liver to hypertrophy before the definitive surgery is carried out to remove the tumour.
As a university surgical unit, we have advanced in the minimally invasive surgical techniques for liver cancer which includes laparoscopic targeted therapies for liver such as radio-frequency ablation and laparoscopic liver resections.
Liver Transplant
The NCIS provides the full spectrum of liver cancer surgery including liver transplants. A liver transplant is a surgical procedure which involves removing and replacing the diseased liver of the patient with a healthy liver from a donor. Most liver transplant operations use livers from deceased donors, though a liver may also come from a living donor.
