Make an appointment or seek a second opinion here.
The urinary bladder is the organ that collects and stores urine made by the kidneys. It is made up of muscle tissue which contracts to expel urine from the body.
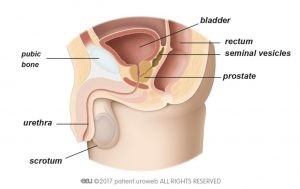
Anatomy of bladder in men
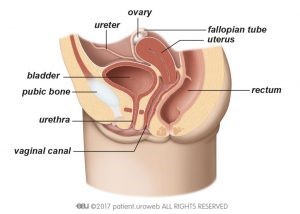
Anatomy of bladder in women
Our bodies are made up of cells which constantly divide and regenerate to make new cells. It is not fully understood why, but when abnormal cells keep dividing, they eventually form a lump of tissue called a tumour. Not all tumours are cancerous. Benign tumours may grow in size but do not spread to other parts of the body unlike malignant tumours which have the potential to spread. Bladder cancer means there are cancer cells inside the bladder that have formed a malignant tumour.
Stages of the disease
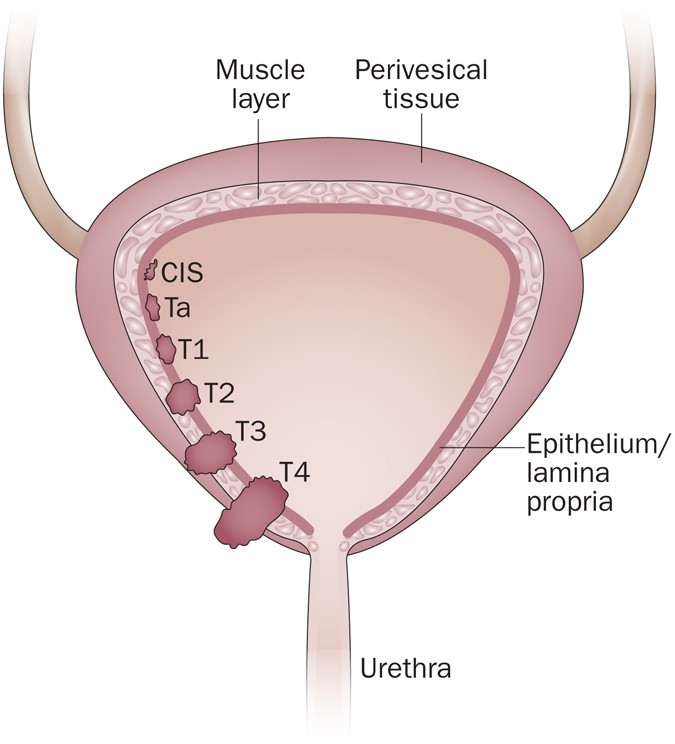
This figure shows the different stages of bladder cancer. Ta and T1 are non-muscle invasive while T2, T3 and T4 are muscle invasive.
A tumour that grows towards the centre cavity of the bladder without growing into the muscle tissue of the bladder is called non-muscle invasive. These tumours represent an early stage. This is the most common type of bladder cancer. In most cases, these tumours are not aggressive and rarely spread to other organs, and can be cured without removal of the bladder.
As the cancer grows into the muscle of the bladder and spreads into the surrounding muscles, it becomes a muscle-invasive bladder cancer. At this stage, the cancer can still potentially be cured with surgical removal of the bladder. This type of cancer has a higher chance of spreading to other parts of the body.
If bladder cancer spreads to other organs, it is called metastatic bladder cancer. At this stage, cure is unlikely, and treatment is limited to controlling the spread of the disease and reducing the symptoms.
* People who think they may be at risk should discuss this with their doctor.
Blood in the urine is the most common symptom of bladder cancer. Non muscle invasive tumours rarely cause pain. Sometimes the only early warning of cancer is the detection of microscopic blood in urinary screening tests.
If you have painful urination or need to urinate more often, a malignant tumour might be suspected, particularly if an infection has been ruled out. A muscle-invasive bladder cancer can cause symptoms as it grows into the muscle of the bladder and spreads into the surrounding muscles.
Symptoms like pelvic pain, pain in the flank, weight loss, or the feeling of a mass in the lower abdomen may be present in some cases when tumours are more advanced.
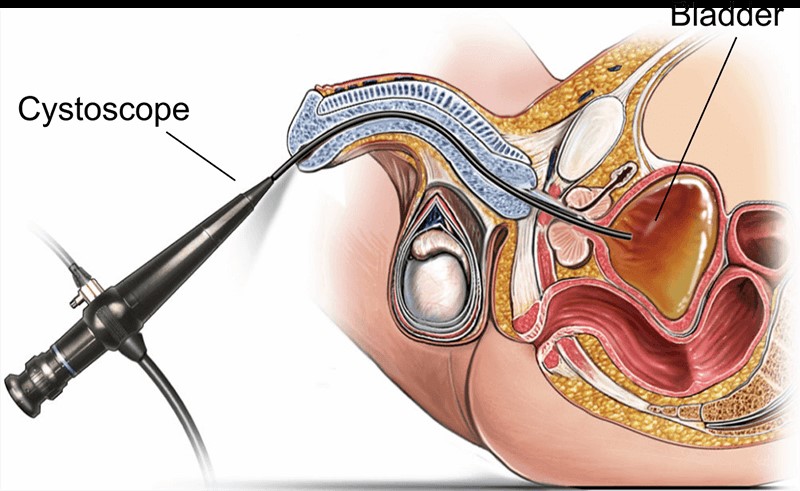
Flexible cystoscopy
Cystoscopy is the main test used to diagnose bladder cancer. It allows your doctor to look at the inside of your bladder and urethra using a thin, lighted tube called a cystoscope. It is performed under local anaesthesia at the urology centre and is an outpatient procedure.
Listed below are the main types of treatment:
Transurethral Resection of Bladder Tumour (TURBT)
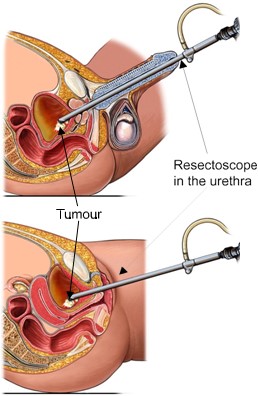
Transurethral resection of bladder tumour (TURBT)
TURBT is a minimally invasive removal of bladder tumours. This procedure is both diagnostic and therapeutic. It allows for examination of the tumour under a microscope and also allows for the complete removal of all visible tumours. In some cases, a second TURBT is required after several weeks to ensure that the cancer has been completely removed and that the initial staging was accurate. TURBT can eradicate non muscle invasive bladder cancer.
Intra-vesical immunotherapy (BCG)
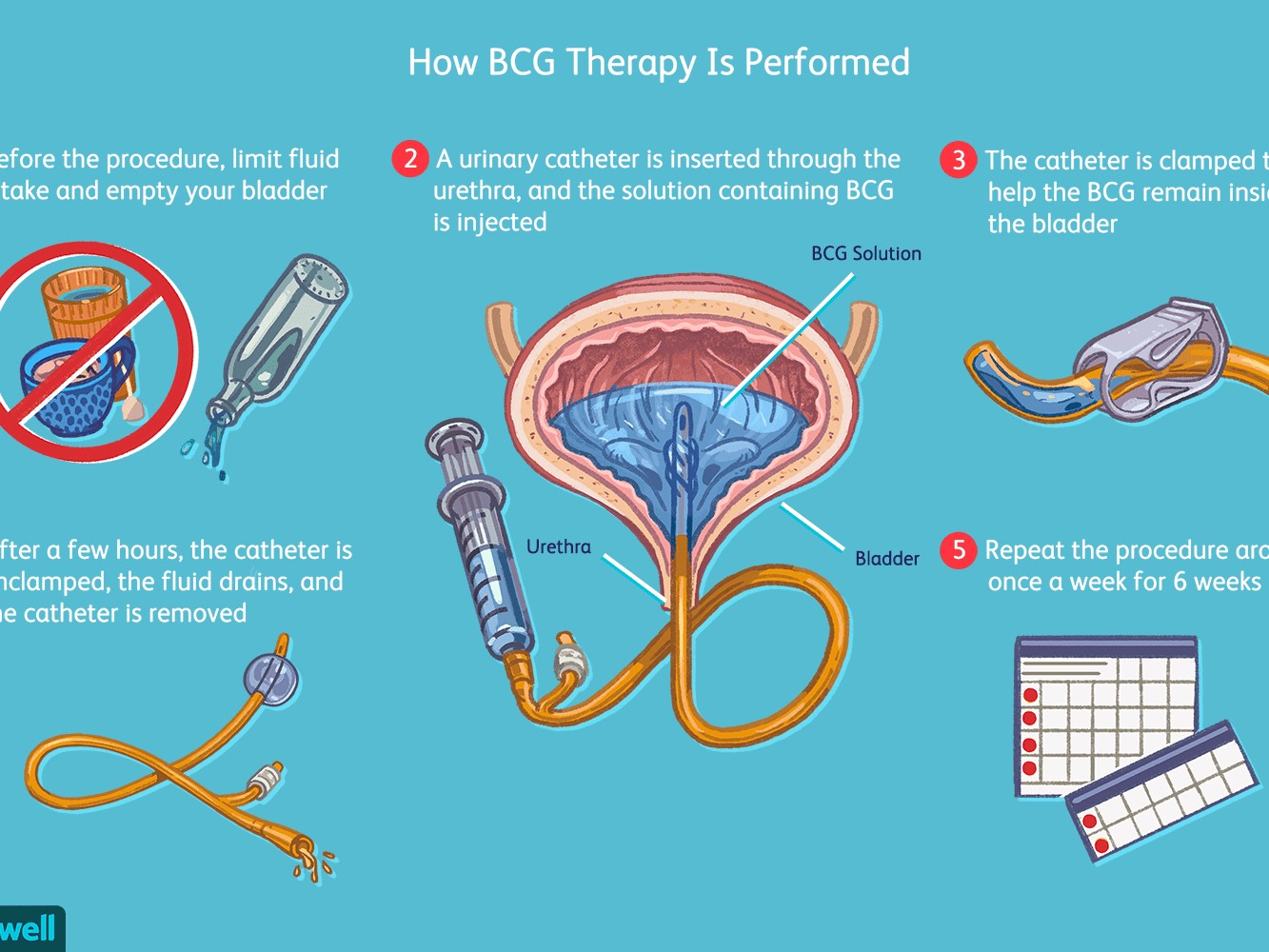
TURBT can eradicate non-muscle invasive bladder cancer. However, there is a still a possibility of recurrence (cancer returning) within the bladder. The chance of recurrence can be reduced by instilling medications within the bladder several weeks after completion of TURBT. This medication is called Bacillus-Calmette Guerin (BCG), a live but weakened bacteria, similar to the BCG used in Singapore's national vaccination programme against tuberculosis. The BCG bacteria is placed as a solution into the bladder through a urinary catheter. This BCG causes inflammation of the bladder wall which in turn stimulates the immune system to kill any cancer cells which may be present in the bladder. The drug itself stays in your bladder for two hours and is then drained out through the urinary catheter, or leaves your bladder when you pass urine. The recommended number of sessions of BCG instillation depends on the aggressiveness of the original bladder cancer but most patients would receive at least 6 weekly sessions and a booster of 3 weekly sessions 3 months later. Your urologist will advise you accordingly.
Cystectomy (removal of the urinary bladder)
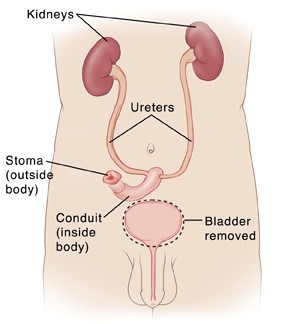
The mainstay of treatment to cure muscle-invasive bladder cancer is the surgical removal of the urinary bladder. The urinary bladder is removed through open surgery. A segment of small intestine is used to create a conduit (pouch) to collect urine from the kidneys. This pouch drains urine out of the body through an opening created in the abdominal wall called a stoma. In selected cases, the small intestine can be used to create a new urinary bladder (neobladder) which allows patients to urinate through the urethra.
Radiotherapy
Radiation therapy is an option for preserving the bladder in patients who are not candidates for surgery or who do not want surgery. Results from radiotheraphy alone are worse than those from complete removal of the bladder, but if combined with chemotherapy (chemoradiation), acceptable results can be achieved. Side effects include mild to strong irritation of the bladder and digestive tract as well as blood in the urine or stools, incontinence, increased risk of infections, and fistulas (abnormal passages that develop between organs).
Follow-up after treatment for bladder cancer
After any kind of cancer treatment follow-up is essential. If the bladder has not been removed, regular cystoscopy is recommended to detect any recurrence of cancer early. Regular scans will also be arranged to ensure that cancer does not return in other organs, lymph nodes or in the kidneys and ureters.