NUHS Institutions will NEVER ask you to transfer money or disclose bank details over a call.
If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg.
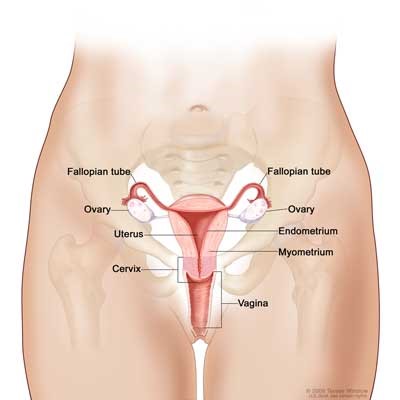
Endometrial cancer or sometimes also known as uterine cancer is the most common gynaecological cancer in Singapore women with rising incidence. Endometrial cancer (uterine cancer) is a type of cancer that begins in the uterus. The uterus is the hollow, pear-shaped pelvic organ in women where fetal development occurs. Endometrial cancer (uterine cancer) begins in the layer of cells that form the lining (endometrium) of the uterus.
Endometrial (uterine) and ovarian cancers are common in women who work and live in an urban environment where they are likely to have fewer pregnancies, breastfeed less and are more likely to have conditions such as obesity and diabetes. These factors alone do not explain why women get endometrial cancer, but they are factors that are more commonly found in women who have endometrial cancer.
The endometrium is the lining of the womb or uterus. It is into this lining that the very early foetus or embryo implants and continues to grow, making the uterus its home for the nine months of pregnancy till birth. This important tissue layer changes over entirely every single month, growing in anticipation of a pregnancy then shedding when no pregnancy occurs.
Cancerous changes in the lining of the womb typically take place in a woman’s late 40s and cancer of the endometrium is most commonly diagnosed in women in their 50s and 60s.
The one very bright star in the dark night of an endometrial cancer (uterine cancer) diagnosis is that >70% of cancers are diagnosed in the very first stage of development, also known as FIGO Stage I. Unlike ovarian cancer, most women with endometrial cancer (uterine cancer) are found to have their disease before it has a chance to spread outside of the uterus. This is because even early or pre-cancerous changes in the endometrial lining will result bleeding that most women will know to be “abnormal”. Because there are troublesome signs that appear early, most women will see a doctor, make the diagnosis and get timely treatment. This is why endometrial cancer (uterine cancer) is unlikely to be deadly although it is a very common gynaecological cancer.
You can beat endometrial cancer (uterine cancer), most women do. All it takes is the courage to get tested if you have troubling symptoms, get treated and move on with your life and endometrial cancer (uterine cancer) need not trouble you again for the rest of your days.
*People who think they may be at risk should discuss this with their doctor.
*People who think they may be at risk should discuss this with their doctor.
Endometrial cancer (uterine cancer) can only be diagnosed after a tissue sample has been removed from the uterine lining and examined in the lab. This uterine tissue sample is most commonly obtained via an office procedure known as an endometrial sampling or a minor procedure performed in the operating theatre known as dilation and curettage or D&C.
Endometrial sampling is carried out almost the same way as a Pap smear, in the office and without the need for anesthesia. The entire procedure typically takes around 5-10 minutes. A fine straw-like device is passed into the uterine cavity and a small sample of the uterine lining is sucked out and sent to the lab for analysis and testing. Women who undergo this simple office procedure can expect some menstrual-like cramping during the procedure and in the few hours following the procedure. There may also be some light spotting for a day or two after the procedure. The main advantage of this procedure is that there is no need to undergo general anesthesia which makes the procedure most likely to be recommended by your doctor.
Dilation and curettage or D&C is a day surgical procedure. Women who undergo this procedure will need to be admitted to the hospital and can expect to stay a few hours without the need for an overnight stay. This procedure typically takes around 15-30 minutes and is performed under general anesthesia where the patient is completely asleep during the procedure. Women will typically experience some mild cramping and light bleeding after the dilation and curettage procedure for up to three days. The dilation portion of the procedure refers to the process where the cervix or neck of the womb is gently widened to allow the curette to pass into the uterine cavity. The curettage portion of the procedure is where the curette is used to gently scrape or curette the uterine lining for samples that can be tested. The process of dilation and curettage can be uncomfortable which is why it is typically performed under general anesthesia with the patient completely asleep.
Depending on the stage of endometrial cancer (uterine cancer), there are various treatment options available.
Stage I
Cancer is confined to the uterus only.
Stage II
Cancer is present in both the uterus and the cervix.
Stage III
Cancer has spread beyond the uterus, but hasn't reached the rectum and bladder. The pelvic area lymph nodes may be involved.
Stage IV
Cancer has spread past the pelvic region and can affect the bladder, rectum and more distant parts of the body.
Most women with endometrial cancer (uterine cancer) are productive members of society. Women living with endometrial cancer (uterine cancer) are mothers, grandmothers, bus drivers, entrepreneurs, policewomen and CEOs, they could be your colleague or the confident woman in a business suit standing next to you on the morning commute. Women living with endometrial cancer (uterine cancer) are unaffected by their disease. This is because even very early changes in the endometrium can result in unusual vaginal bleeding patterns as described above. This usually prompts women who have vaginal bleeding that is unexpected to see their gynaecologist or primary care doctor who helps make the diagnosis of endometrial cancer (uterine cancer).
Endometrial cancer (uterine cancer) is treated with surgery. In most women, surgery to remove the uterus, ovaries and Fallopian tubes is sufficient to treat endometrial cancer (uterine cancer) completely. Depending the size of the tumour and other characteristics of the endometrial cancer (uterine cancer), additional tissues surrounding the uterus such as lymph nodes and the omentum may need to be removed during surgery as well. Only women who are then found to have cancer outside of the uterus or who are at risk for cancer cells remaining in the body are given the recommendation to have further treatment in the form of radiation therapy, most commonly, or a combination or chemotherapy and radiation, rarely. About 90% of women with endometrial cancer (uterine cancer) will require no treatment beyond surgery.
Cancer is a complex condition and knowledge about cancer and cancer treatment is constantly changing and getting more sophisticated to deliver ever better patient outcomes. The very best cancer care is therefore best delivered by a team of professionals, with each member of the team being an expert in their own field but working TOGETHER to take care of the whole person.
At the NCIS, we believe that when we treat the WHOLE PERSON, a WHOLE PERSON walks out our doors. This is the philosophy and thinking that lies at the heart of our Whole Person Approach to Endometrial Cancer (Uterine Cancer) Care at the NCIS.
How the NCIS Helps Keep You and Your Loved Ones Safe from Womb Cancer (Endometrial Cancer / Uterine Cancer)
When it comes to surgery in the treatment of endometrial cancer, women who receive their care at the NCIS have had a more contemporary option since 2008 through robot-assisted surgery.
Employing robotic technology, surgeons are able to perform very complex surgical operations without the need to “open up” the abdomen. Open surgery has traditionally been the most effective way to carry out complex cancer surgery, till the introduction of surgical robotics.
From a woman’s perspective, endometrial cancer surgery has always been somewhat puzzling, since women living with endometrial cancer are unaffected by their disease, the treatment in the form of open surgery and its lengthy recovery process, is often viewed as being worse than the disease. This challenge to make the surgical treatment of endometrial cancer (uterine cancer) more efficient and less debilitating is one of the primary concerns to the gynaecological cancer surgical team at the NCIS.
Robotics has helped us take a giant step towards someday treating endometrial cancer (uterine cancer) without any down down or “zero impact treatment”. The following table helps to illustrate just how far we have come at the NCIS in helping our patients get better more efficient cancer surgical care.
| | Open Surgery | Robotic Surgery |
|---|---|---|
| Hospital Stay | 4-7 days | Overnight |
| 90% Recovery | 10 weeks | 10 days |
| Typical Surgical Blood Loss | 300ml | 30-50ml |
If you or a loved one are exploring surgical treatment for endometrial cancer (uterine cancer), consult your Gynaecologic Oncology Team Specialist at the NCIS to see if robot-assisted surgery is right for you.
The Womb Cancer (Endometrial Cancer / Uterine Cancer) Journey @ NCIS
The women we care for may have endometrial cancer (uterine cancer), but the disease is only one part of a whole person who is a living, breathing and feeling entity. Since most women living with endometrial cancer (uterine cancer) are functionally great, the team at the NCIS believes in not only treating cancer but protecting that wonderful, functional and healthy woman inside every endometrial cancer (uterine cancer) patient. Achieving this starts with having a team of dedicated healthcare professionals support each and every aspect of the whole person as we journey with our patients through diagnosis, treatment, recovery and beyond.
The Women’s Emotional Health Service (WEHS)
This team of emotional health specialists are an important component of the endometrial cancer care solution. Quite simply, a fit emotional state ensures a healthy immune system that fights cancer more effectively. Coming to terms with a diagnosis of endometrial cancer can be difficult, especially since most women who’ve been given a diagnosis of endometrial cancer feel so well and so vital. Effective emotional assessment and support is a complex, constantly evolving process and something the Women’s Emotional Health team does exceptionally well, supporting a growing community of healthy, happy endometrial cancer survivors, one woman at a time. Our patients are supported through a combination of CARE therapy, hypnotherapy and medical therapeutics. At the NCIS, we are proud of the important work that our WEHS team does, and our cancer survivors agree!
The Total Lymphoedema Team
Lymphoedema is a complex and potentially debilitating condition that develops as a result of cancer surgery and therapy in some patients, especially in patients who have had lymph nodes removed as part of their endometrial cancer surgery. At the NCIS, we believe that the best treatment is prevention. This belief is embodied in the creation of the Total Lymphoedema Clinic (TLC) to support all the women living with cancer that we care for at the NCIS who may be at risk for lymphoedema. The team at the TLC consists of surgeons, physicians, physiotherapists, nurses and occupational therapists who are all committed to one thing, helping our patients come out of endometrial cancer (uterine cancer) WHOLE and functional with sub-specialty professionalism and Tender Loving Care.
Advanced Practice and Specialty Nursing
At the NCIS, we love our nurses for one very simple reason. Our Advanced Practice and Specialty nurses translate all the expertise available at NUH in to the care that our patients receive. The women living with endometrial cancer (uterine cancer) that walk in our doors walk out whole because of the dedication and professionalism that these cancer professionals show all day, every day. Effective cancer care is an incredibly complex process which our Advanced Practice and Specialty nursing team has the training, education and expertise to understand, coordinate and help deliver to the women receiving care for endometrial cancer (uterine cancer) at the NCIS. It’s no wonder that our cancer survivors hug a cancer specialty nurse wherever they meet one!
The Womb Cancer Treatment Team at NCIS is spearheaded by Professor Jeffrey Low accompanied by his team of medical professionals.
The team is committed to delivering uncompromised and dedicated clinical research, expertise and care in the prevention, management and cure of Womb Cancer.
Gynaecologic Oncology
Medical Oncology
Pathology
Radiation Oncology
Radiology