NUHS Institutions will NEVER ask you to transfer money or disclose bank details over a call.
If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg.
Make an appointment or seek a second opinion here.
Download this patient’s guide to understanding multiple myeloma for potential questions to ask your doctor during consultation.
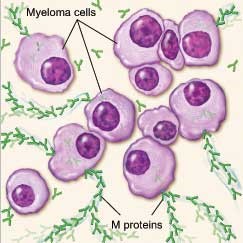
Multiple Myeloma is a type of bone marrow cancer characterised by abnormal expansion of malignant plasma cells in the bone marrow. It is the second most common type of blood cancer and afflicts more than 100 patients in Singapore a year. It has a rising incidence in Asia, the reason for which is still elusive. These tumours may keep the bone marrow from making enough healthy blood cells. Normally, the bone marrow makes stem cells (immature cells) that become three types of mature blood cells:
As the number of myeloma cells increases, fewer red blood cells, white blood cells, and platelets are made. The myeloma cells also damage and weaken the bone.
In time, myeloma cells collect in the bone marrow. They may damage the solid part of the bone. When myeloma cells collect in several of your bones, the disease is called "Multiple Myeloma". This disease may also harm other tissues and organs, such as the kidneys.
Myeloma cells make antibodies called "M proteins". These proteins can collect in the blood, urine and organs.
Eventually, myeloma causes anaemia, lytic bone lesions which may cause bone pain or fractures, renal impairment and hypercalcaemia.
*People who think they may be at risk should discuss this with their Doctor.
*A Doctor should be consulted should the above symptoms occur.
There is currently no way to prevent Multiple Myeloma.
If you have a symptom that suggests Multiple Myeloma, your Doctor must find out whether it is due to cancer or some other cause. Your Doctor may ask about your personal and family medical history. You may also have one or more of the following tests.
Physical Exam
Your Doctor checks general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
Blood Tests
Your Doctor may order blood tests. The lab may check the level of many different proteins, including M protein and other immunoglobulins (antibodies), albumin and beta-2-microglublin as Multiple Myeloma causes high levels of proteins in the blood. The lab may also do a complete blood count to check the number of white blood cells, red blood cells, and platelets as myeloma may also cause anaemia and low levels of white blood cells and platelets. The lab may also check for high calcium levels or perform creatinine tests.
Urine Tests
The lab may test for Bence Jones protein, a type of M protein, in urine. The lab measures the amount of Bence Jones protein in urine collected over a 24-hour period. If the lab finds a high level of Bence Jones protein in your urine sample, Doctors may monitor your kidneys as Bence Jones protein can clog the kidneys and damage them.
X-rays
This test is used to identify lytic lesions in the bones caused by myeloma. In addition, this test can also detect any weakened bone areas or fractures that may require surgery.
Magnetic Resonance Imaging (MRI)
A procedure that uses magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is called nuclear magnetic resonance imaging (MRI). An MRI may be used to find areas where the bone is damaged.
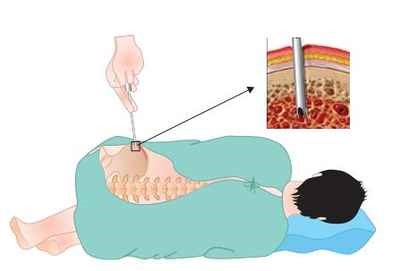
Biopsy
The Doctor may remove tissues to look for cancer cells. A biopsy is the only sure way to know whether myeloma cells are in your bone marrow. Before the sample is taken, local anaesthesia is used to numb the area to help reduce the pain. The doctor then removes some bone marrow from your hip bone or another large bone. A pathologist uses a microscope to check the tissue for myeloma cells. There are two ways the doctor can obtain bone marrow. Some patients may encounter both procedures during the same visit.
There are different treatments available for Multiple Myeloma depending on the stage of Multiple Myeloma. Factors other than the stage of cancer that might have an impact on your treatment decision include your age, your overall health, and your own preferences. The three main types of treatment include:
Watchful Waiting
People with smoldering myeloma may be able to put off having cancer treatment. By delaying treatment, you can avoid the side effects of treatment until you have symptoms.
If you and your Doctor agree that watchful waiting is a good idea, you may have regular checkups (such as every 3 months) and receive treatment if symptoms occur.
Although watchful waiting avoids or delays the side effects of cancer treatment, this choice has risks. In some cases, it may reduce the chance to control myeloma before it gets worse.
You may decide against watchful waiting if you don’t want to live with untreated myeloma. If you choose watchful waiting but grow concerned later, you should discuss your feelings with your Doctor.
Induction Therapy
Many different types of drugs are used to treat myeloma. People often receive a combination of drugs, and many different combinations are used to treat myeloma.
Each type of drug kills cancer cells in a different way:
You may receive the drugs orally or through a vein (IV). The treatment usually takes place in an outpatient part of the hospital, at the Doctor’s office, or at home. Some people may need to stay in the hospital for treatment.
Stem Cell Transplant
Many people with Multiple Myeloma may get a stem cell transplant. A stem cell transplant allows you to be treated with high doses of drugs. The high doses destroy both myeloma cells and normal blood cells in the bone marrow. After you receive high-dose treatment, you receive healthy stem cells through a vein. New blood cells develop from the transplanted stem cells so they can replace the one that were destroyed by treatment.
Stem cell transplants may take place in the hospital or in the outpatient setting. Patients will be assessed individually for suitability for either setting. Some people with myeloma have two or more transplants.
Stem cells may come from you or from someone who donates their stem cells to you:
There are two ways to get stem cells for people with myeloma. They usually come from the blood (peripheral blood stem cell transplant). Or they can come from the bone marrow (bone marrow transplant).
After a stem cell transplant, you may stay in the hospital for several weeks or months. You’ll be at risk for infections because of the large doses of chemotherapy you received. In time, the transplanted cells will begin to produce healthy blood cells.

Multiple Myeloma Care Approach

Multiple Myeloma Care Team

Multiple Myeloma Online Resource Library

Patient Support Groups

Multiple Myeloma Clinical Trials
Multiple Myeloma Resesarch